What is respiratory failure?
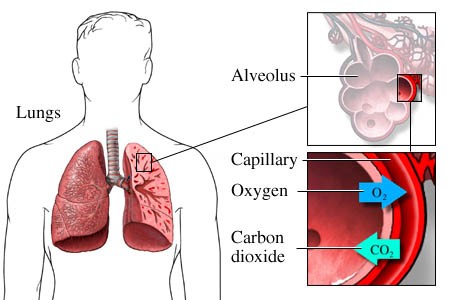 The main function of our lungs is to get oxygen into the body and to release carbon dioxide. The lungs allow gas exchange to happen, moving oxygen into the body and carbon dioxide out of the body. Respiratory failure occurs when the respiratory system fails to provide the body with adequate amounts of oxygen and/or fails to remove the carbon dioxide.
The main function of our lungs is to get oxygen into the body and to release carbon dioxide. The lungs allow gas exchange to happen, moving oxygen into the body and carbon dioxide out of the body. Respiratory failure occurs when the respiratory system fails to provide the body with adequate amounts of oxygen and/or fails to remove the carbon dioxide.
This page focuses on type 2 respiratory failure, which is where the carbon dioxide is not removed sufficiently from the body.
What are the symptoms of type 2 respiratory failure?
People may experience a number of symptoms including:
- severe headaches not relieved by pain killers
- drowsiness
- confusion
- unusual jerking or shaking.
The onset of symptoms can be sudden (acute) or can happen more slowly (chronic).
How is type 2 respiratory failure diagnosed?
Type 2 respiratory failure can be diagnosed from a blood test. In hospital, this is usually done by an arterial blood gas sample, where a sample of blood is commonly taken from the artery in your wrist. In the community, we use capillary testing where a small amount of blood is taken from your ear lobe.
How is type 2 respiratory failure treated?
This is an excess of carbon dioxide in your blood. This build-up of carbon dioxide is due to the lungs being unable to clear it sufficiently from the body. This may be due to an infection or may be due to diseases, such as chronic obstructive pulmonary disease (COPD). In some cases people compensate for these high levels of carbon dioxide and can be monitored and managed at home. It is important for those who care for you to know that you have had or have type 2 respiratory failure. Your nurse will discuss this with you.
If the body is no longer able to compensate then you may become extremely unwell and hospital admission may be required. You may be treated with therapy called non- invasive ventilation (NIV), sometimes referred to as bi-level positive airways pressure (BiPAP), to help the body get rid of the carbon dioxide. In some cases, this treatment may be carried out long-term at home and will require referral to chest specialists to allow you to discuss further treatment and to monitor you when you are on it.
If you need non-invasive ventilation (NIV), masks and equipment are available at the William Harvey Hospital in Ashford.
01233 633331 extension 86193.
You may be able to purchase support and/or products to help with obstructive sleep apnoea (OSA) from Philips Respironics: Management of Specialist Therapy (MOST).
0800 652 0303
sleepapnoea.respironics.co.uk
Contact us
Please contact your respiratory nurse, community nursing team or GP if you have any of the following symptoms:
- severe headaches not relieved by pain killers
- drowsiness
- confusion
- unusual jerking or shaking.